Different optical designs
Background

The IOLs available in the past were largely hard plastic lenses made of PMMA (commonly known as "Plexiglas"). The underlying optical design consists of two identical (symmetrical) purely spherical surfaces. This type of lens is the most commonly used in optics, as it is technically comparatively simple and therefore inexpensive to manufacture.
However, these classic IOLs have two major disadvantages:
- large incisions during implantation as these IOLs are rigid
- considerable imaging errors(spherical aberration), especially with high refractive powers

In order to eliminate these disadvantages, a large number of new types of lenses have been developed in recent years. The trend is towards very thin, foldable IOLs that can be implanted minimally invasively through incisions of just 1.5 mm to 3 mm. For implantation, so-called cartridges are often used, narrowing plastic tubes through which the previously folded IOL can be implanted through this miniature incision using a special pen (so-called injector). In a large study, the effects of these injection processes, some of which place considerable stress on the IOL material, were examined in detail at the ITIV in collaboration with the Eye Clinic at the University of Ulm.
Imaging quality

The so-called optical imaging quality is decisive for the optical function of the IOL and thus for the best possible vision of the patient. This is essentially determined by the geometry of the surfaces and their surface quality (e.g. roughness due to the manufacturing process). In the case of IOLs, a distinction can be made between four basic types, which are described in more detail below: symmetrical spherical, asymmetrical spherical, aspherical and bifocal or multifocal (often also diffractive) designs.
MTF systemTo measure these imaging properties of IOLs, a special measuring system has been developed at the Institute which makes it possible to determine the imaging properties and thus the optical quality of monofocal and multifocal IOLs extremely precisely. The measurement is carried out in accordance with the international industry standard EN/ISO 11979-2 [ISO11979]. According to this standard, a special artificial eye is used to test the IOL under measurement conditions that are similar to those that will later be used in the eye, simulating the properties of the cornea and the anterior chamber. The IOL itself is operated in a special water bath. Further detailed information on how the IOL measuring stand works can be found here.
Symmetrical spherical designs
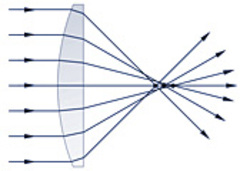
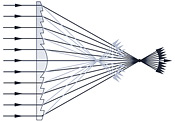
Although spherical surfaces (sections of spherical surfaces) are technically comparatively easy and therefore inexpensive to produce, they have a significant fundamental imaging error, the so-called spherical aberration. The reason for this is that a sphere (or, as shown here, a circle viewed in section) is not the optimum geometric shape for perfect imaging (focusing of parallel rays) [Hecht98], [Charman96]. As can be seen from the adjacent figure, rays close to the optical axis (so-called paraxial rays) are focused further away from the lens than rays from the outer areas of the lens. This leads to a suboptimal, blurred focus or a blurred image.
All spherical designs exhibit this imaging error, which is largely dependent on the diameter of the incident light beam (the so-called entrance pupil). For small diameters, i.e. in the eye with small pupil sizes (opening of the iris), the spherical aberration becomes increasingly smaller. The majority of intraocular lenses are currently implanted in patients over the age of 60. The ability of the iris to vary its opening diameter decreases significantly with age. While small children achieve pupil openings of up to 6mm or even 8mm, the average pupil opening in older people is 3mm to 4mm (approx. 3mm under normal lighting conditions). For this reason, for example, the industry standard for testing IOLs (EN/ISO 11979-2 [ISO11979]) specifies a pupil size of 3mm.
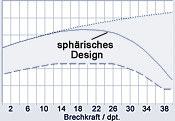
With such small pupil openings, however, significant spherical aberrations only occur with comparatively large refractive powers. The adjacent graph shows the dependence of the image quality (ISO criterion, modulation at 100 line paren/mm, see also image quality) on the refractive power (in diopters, dpt.) of the IOL with a pupil opening of 3mm. The solid curve in the middle area shows the image quality of the classic symmetrical spherical design. The dotted (upper) curve, on the other hand, shows the theoretically achievable maximum values of an ideal (so-called diffraction-limited) lens, while the dashed (lower) curve shows the minimum values of image quality required by the industry standard [Rawer05a]).
It can be clearly seen that with this pupil opening, spherical aberrations only become noticeable from a refractive power of approx. 15dpt. Up to a refractive power of approx. 25dpt. the image quality remains largely constant, although the theoretical maximum is no longer reached. At refractive powers above 25dpt. the image quality of symmetrical spherical IOLs drops significantly. For low refractive powers, symmetrical spherical IOLs are therefore perfectly acceptable for the average patient. For large refractive powers or for patients with larger than average iris openings or for younger patients, however, a considerable reduction in visual acuity is to be expected. For these patients, the designs described below can provide a remedy.
Asymmetric spherical designs
The imaging errors of spherical surfaces (so-called spherical aberration) can be reduced with a simple trick: The proportions of the refractive forces (deflection of the rays) of the two surfaces must be distributed as evenly as possible.
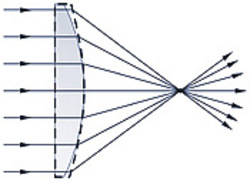
The background to this is the fact that spherical aberration increases disproportionately with a greater angle of deflection. If the plano-convex lens (lens with a flat boundary surface and an outwardly curved boundary surface) is simply reversed in the beam path compared to the example shown above, the spherical aberration is significantly smaller, as the flat surface now also contributes to the refraction.
So-called. Lenses of the best shape make optimum use of this effect for a defined (typical) beam path. For typical use in the eye, the second surface is also slightly curved, but much less so than the first.
In practice, however, a potential source of error must be taken into account for all asymmetric IOLs, which can have dramatic effects on the optical function of the IOL: The orientation of the IOL must be maintained correctly, otherwise the principle optical advantages of an asymmetric spherical design can turn out to be the exact opposite. This means that it must be ensured that the front and back of the IOL are not interchanged during implantation under any circumstances [Spraul05]. If, on the other hand, the anterior and posterior surfaces are reversed, a lens with the best shape becomes a lens with a very unfavorable shape, which has even worse imaging properties than a simple symmetrical spherical design.
However, the actual reason for using asymmetrical spherical lens designs in the field of intraocular lenses is usually the desire to achieve a constant thickness (so-called center thickness) for foldable IOLs, as otherwise lenses with a higher refractive power would be considerably thicker than those with a lower refractive power. A uniform thickness of the lens leads to significantly improved manageability of the different lenses during minimally invasive implantation with or without injector systems.

However, as can be seen in the diagram above, this leads to a smaller effectively usable optical surface (or iris opening), as the upper surface has an approx. 15% smaller diameter than the lower one. Our measurement results also show that the commercially available asymmetric spherical IOLs examined often achieve only insignificant improvements in image quality. Thus, the basic optical advantages of such an asymmetric design are often not fully utilized.
Aspheric designs
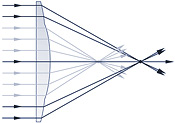
In order to completely eliminate the spherical aberrations described above, non-spherical or aspherical surfaces must be used. These must have a lower curvature in the outer areas than in the central area. In this way, an optimum focus and therefore optimum imaging properties of the IOL can be achieved. Such aspheric IOLs can guarantee optimal imaging properties even with high refractive powers and large pupil openings and therefore offer the best imaging properties for the patient in principle and therefore the best conditions for maximum visual acuity after implantation.
Aspheric aberration-corrected designs
Recently, another variant of aspheric lenses has been propagated. While the cornea of the eye was assumed to be purely spherical in the classical design, the results of modern and increasingly precise measuring systems for measuring the surface of the cornea [Brennan97] show that this is also not purely spherical, i.e. also aspherical. In order to take this fact into account, so-called 'abberation-corrected' IOLs have recently been offered, the design of which takes into account the average asphericity of the cornea. This enables improved vision on average for the patient population. However, in order to be able to guarantee this advantage to every patient, the exact asphericity would have to be measured and a suitable IOL selected.
For measurements according to ISO11979, however, a purely spherical artificial cornea is specified. Accordingly, aberration-corrected aspheric lenses tend to perform slightly worse in these measurements than non- aberration-corrected aspheric lenses. However, this is not representative for the in vivo use of aberration-corrected IOLs, as the measurement setup according to ISO11979 does not take this statistical asphericity of the human cornea into account.
Measurements with a modified measurement system, which uses a corresponding aspheric artificial cornea, will therefore be submitted at a later date.
It should also be mentioned that a Strehl ratio greater than 0.90 is generally far superior to the other optical components of the human eye and therefore only rarely helps the patient to achieve a subjective improvement in visual acuity.
Bifocal/mutifocal designs

A major disadvantage of previous artificial IOLs is that they are monofocal lenses with a fixed refractive power. This means that patients largely lose their ability to accommodate. As a rule, the refractive power of the IOL is therefore selected so that the patient can see clearly at a distance (e.g. for driving) without additional glasses. For near vision (e.g. reading), however, the patient needs reading glasses. However, as the natural ability to accommodate decreases significantly with age, older people generally need reading glasses anyway. Therefore, for many patients, this limitation is quite acceptable.

This disadvantage of only being able to see clearly at one distance can be largely eliminated with so-called multifocal or bifocal lenses. This type of lens produces two different focal points simultaneously. This means that close objects (e.g. when reading) and distant objects (e.g. when driving) can be focused on at the same time. Reading glasses are therefore generally superfluous.

The disadvantage of this type of lens, however, is that the eye not only always perceives two sharp images at the same time, but also two blurred overlaid images. This leads to a slight decrease in image sharpness compared to a monofocal lens. However, as bifocal IOLs often use aspherical surfaces and therefore have otherwise excellent imaging properties, studies show that the image quality of a good bifocal lens is equal to or even better than that of a classic IOL with a clear spherical aberration. In addition, so-called glare effects can occur (e.g. when driving at night, when car headlights appear at the edge of the field of vision in an otherwise very dark environment, or when the patient is dazzled by oncoming vehicles) [Akutsu93]. In these cases, fine geometric patterns may become visible, e.g. slight concentric rings superimposed on the actual image. In rare cases, these are perceived as disturbing by the patient.
With these bifocal designs, a distinction can be made between two basic design variants:
One is the simpler variant, which has been available on the market for years, albeit with only moderate success. Here, the lens is divided into a few zones with different refractive powers. In the example diagram above, two such zones can be distinguished: in the central area, for example, a high refractive zone with a focus close to the lens, and in the outer area a low refractive zone with a focus further away from the IOL. The optical designs of the individual zones can in turn be spherical or aspherical, which in turn has an effect on the imaging quality in the same way as monofocal IOLs. The bifocal multi-zone designs currently available on the market usually consist of three to five such zones.
Thedisadvantage of this multi-zone design is that the intensity of the two foci depends on the pupil opening. In the example above, only the closer of the two foci would be pronounced with a small pupil opening (e.g. daylight) and therefore only near vision (e.g. reading the newspaper) would be possible, which can lead to a loss in the suitability of this IOL design for everyday use.
The second variant has emerged with the perfection of high-precision diamond lathes, which can now be used to manufacture IOLs. An additional microstructure, a so-called diffractive structure, is applied to the surface of the IOL. This causes a diffraction of the light (similar to the diffraction effects on the double slit or on grating structures) which is superimposed on the refraction. In this way, the entire surface can be used to generate both focal points (the dependence on the pupil size is thus eliminated), and the imaging quality can be additionally improved with an optimized design.
Accommodative designs
The ideal IOL would, of course, be a lens that simultaneously has ideal imaging properties and enables accommodation. Accordingly, many companies are researching and developing such an accommodative IOL. This would mimic all the functions of the young natural IOL and could theoretically even significantly surpass its optical quality.
So far, however, the availability of such accommodating IOLs is still extremely limited and their function is highly controversial. As soon as this changes, we will extend our comparative measurements to this type of lens.
Contact
Prof. Dr. rer.nat. Wilhelm Stork,
Tel. 0721 / 608 - 2510, wilhelm.stork∂kit.edu

